
Did you know that it’s estimated upwards of 80% of menstruating women experience pain associated with their period? The most common complaint of pain being in the lower belly. BUT, a significant portion of people also experience low back pain during their period. Menstrual cycle associated low back pain is common in the first 4-7 days of your cycle.
Believe or not… period pain is not something that people should have to put up with. In fact, period pain and associated low back pain can indicate something more is going on. Too often people think that their pain is just part of the norm, not something deserving of mentioning at the osteopath or GP. The simple matter is, if you are having lots of pain, cramping, back pain, or otherwise there is options out there to help.
Let’s break down what period pain is. It’s not the most well-defined symptom, because of this it can be hard to put a name to what you are experiencing. The main way of breaking it down is by three categories. The first is called menstrual cramping. This is the kind of pain that falls within “normal” for most people. It’s pain that is felt in the lower abdomen during the first few days of your cycle. Typically speaking, these cramps can be managed well and don’t interrupt daily life.
The second and third categories are a more severe form of menstrual cramping, and they are called primary and secondary dysmenorrhoea. Primary refers to when there is no known reason for the severe pain, this usually happens in younger people (under 25 years old). Secondary dysmenorrhoea refers to when there IS a physical reason for the increased pain. It can be for multiple reasons though including endometriosis and fibroids which we discuss further down.
The main difference between menstrual cramping and dysmenorrhoea is that the pain can significantly impact someone’s life. It can lead to people needing to take sick days off school or work. Not being able to partake in social activities. Even financially it can be costly each month to get pain medication and other medical help.
Dysmenorrhoea is more than just pain in the lower belly. It can cause widespread pain extending into the low back, hips, and even thighs. But WHY does it affect so many tissues?
During menstruation, the body releases hormone-like lipids called prostaglandins. These travel to the uterus and start the contractions to help shed the endometrial lining. It’s these contractions that we feel during cramps. When they are particularly large and significant, they can start to radiate to the back.
One of the reasons for this travelling pain comes down to the nerve supply. You may have also heard of it as referred pain. This means that while there is a dysfunction in one area, we feel it in another due to a shared nerve supply. A classic example of this is shoulder pain during a heart event. Essentially the nerve supply to the uterus is from the low back, so naturally the referred pain can be felt in the low back and legs where the nerve supply is shared.
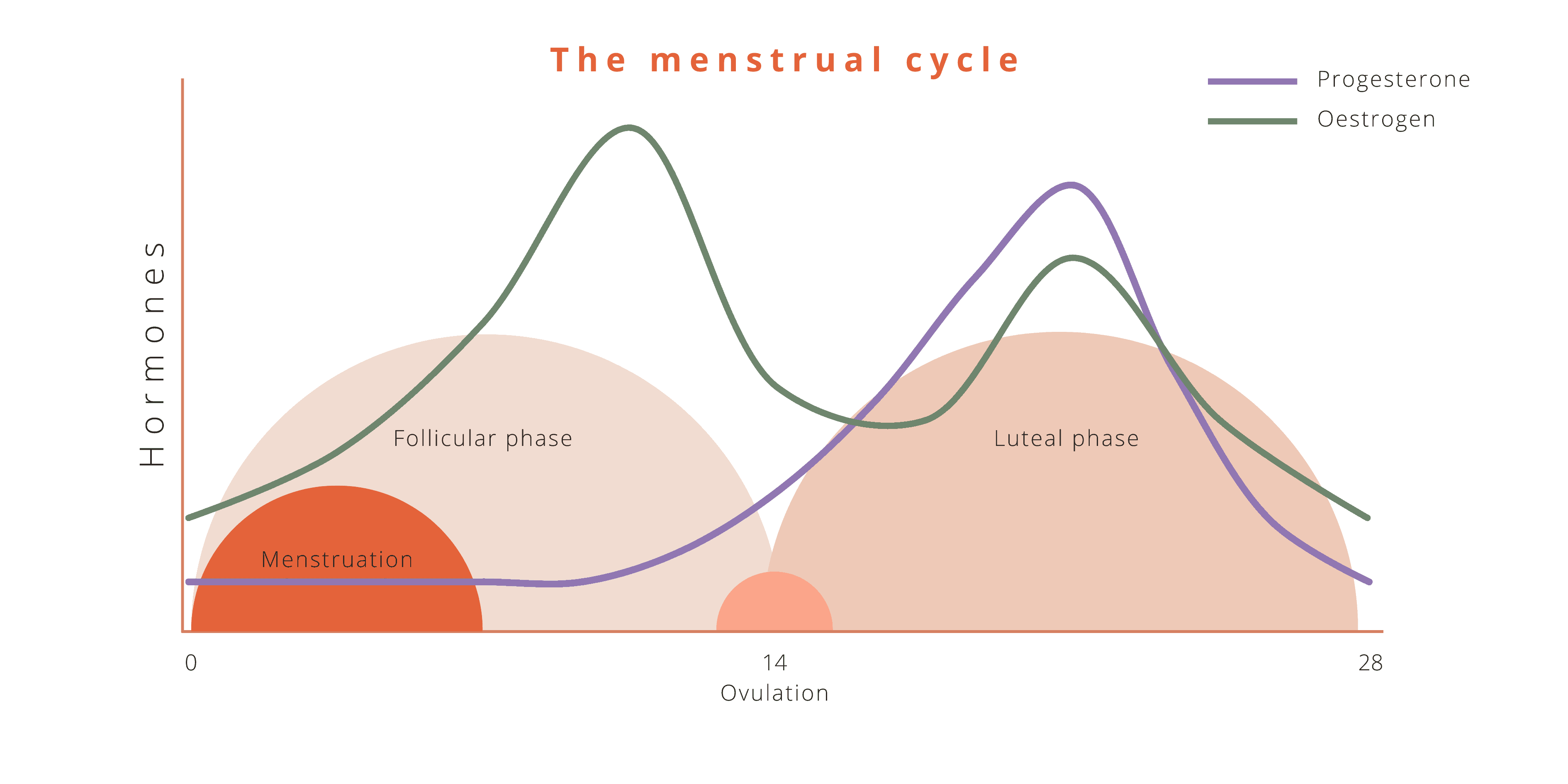
Another thing to note is that during menstruation there is a reduction in oestrogen levels (see table below). This also leads to a weakening of the pelvic floor. The pelvic floor is a major support system to the bladder, uterus, bowels, and helps with stabilisation of the trunk. If there is a dysfunction in these tissues, it can mean there is some added pressure on the muscles and joints in the back causing them to become sore.
Premenstrual syndrome (PMS) and Premenstrual Dysphoric disorder (PMDD)
This is probably something you may have already heard of. PMS refers to a set of symptoms that happen at the end of the luteal phase and in the lead up to your next cycle. It’s very common and can occur in about 3/4s of the population )
It can include symptoms like mood swings and irritability, feeling menstrual cramping, bloating, tiredness, even low back pain! You might also notice changes to your daily routine including appetite changes and sleep changes.
PMDD is fairly similar to PMS although a more severe version. Where most people with PMS are able to get through their daily life without much interference, people with PMDD might struggle with their normal routines.
Endometriosis is the growth of the uterine lining (the endometrium) outside of the uterus. Unfortunately, the research hasn’t been able to show us WHY this happens yet – we have some theories but nothing solid yet. Adenomyosis is the growth of the endometrium into the uterine tissue itself. Both conditions can lead to really debilitating periods for those who have them.
The symptoms can include:
Uterine fibroids are growths of tissue in the muscle wall of the uterus, they are non-cancerous but can still pose of problem for those that develop fibroids. Unfortunately, they can impact daily life significantly causing issues like dysmenorrhoea, menorrhagia, infertility, and bleeding outside of the normal menstrual cycle. They can be painful and can also start to impact other structures like the bladder and bowel as they grow.
Polycystic ovarian syndrome is a hormonal condition which affects the whole body. It gets its name from the effect on the ovaries, where it causes multiple cysts to form. Being a whole body and hormonal condition, it can have widespread symptoms. This can include dysmenorrhoea and irregular periods, excessive body hair, acne, hair loss, infertility, and mood changes.
Osteopathy is a tool that can be used to manage menstrual pain and related low back pain. Osteopaths are highly skilled and trained with a variety of techniques they can use in the treatment of menstrual pain and low back pain. Our understanding of the body and the effects that your menstrual cycle and related conditions can have on the body means we can tailor treatment to your needs. We will look at the whole body, particularly the lower back and pelvis and work on softening any tight tissues that are restricting movement, we can also work on mobilising stiff joints and think about the innervation of the uterus and how that can affect other structures. Osteopaths can also use their knowledge to help you in other ways too, taking you through at home strategies to try and ease your pain. Things like exercise, stretching, or other tips and tricks!
That’s what we do at Boroondara Osteopathy and we’d love to help you out.
Exercise is a great tool to use for helping relieve low back pain during your cycle. Osteopaths can teach you all about exercise and even prescribe exercises that can be used at home to help reduce pain. We consider why the body is sore, what is tight and what may need strengthening. This is different for everyone, so osteopaths take a tailor approach to your care adjusting to your body’s individual needs! We can take you through Yoga based movement practice, pilates, or even general exercise. We work with what you need AND what you enjoy as this is a really important step too!
Some of the conditions we’ve discussed are best managed with a team of people including a GP or other medical doctors. If you are having severe persistent pain and other issues related to menstruation or fertility, checking in with your doctor is a great next step. They’ll be able to help diagnose the issue and manage your condition. Our osteopaths love working with your doctors to come up with the best plan to help manage your pain and/or condition. Managing conditions with a team of practitioners means we can each target different aspects and help you reach your goals.
Low back pain can be a sign of early pregnancy, some people also experience light spotting during the early stages of pregnancy. In these cases, it would be easy to assume the low back pain was just another case of PMS or otherwise menstrual related pain. Our biggest recommendation to you is if it’s not within your normal it’s a good time to check-in with a doctor. OR if there’s a chance you could be pregnant take a quick home test. If you are pregnant and wondering about low back pain, you can find out more by going HERE
Resources
Kaganov, H., & Ades, A. (2016). Uterine fibroids: Investigation and current management trends. Australian Family Physician, 45(10).
Li, Q., Huang, J., Zhang, X., Feng, W., Hua, K. (2021). Dysmenorrhea in patients with adenomyosis: A clinic and demographic study. Journal of Gynecology Obstetrics and Human Reproduction, 50.
Micussi, M. T., Freitas, R. P., Angelo, P. H., Soares, E. M., Lemos, T. M., & Maranhao, T. M. (2015). Is there a difference in the electromyographic activity of the pelvic floor muscles across the phases of the menstrual cycle? Journal of Physical Therapy Science, 27(7), 2233-2237.
Righarts, A., Osborne, L., Connor, J., & Gillett, W. (2018). The prevalence and potential determinants of dysmenorrhoea and other pelvic pain in women: a prospective study. An international Journal of Obstetrics and Gynaecology, 125, 1532-1539.
Ruffini, N., D/Alessandro, G., Pimpinella, A., Galli, M., Galeotti, T., Cerritelli, F., & Tramontano, M. (2022). The Role of Osteopathic Care in Gynaecology and Obstetrics: An Updated Systematic Review. Healthcare, 10.